Uterine Fibroids: Exploring Uterine Fibroid Embolization as an Alternative to Hysterectomy
Uterine fibroids are noncancerous growths of the uterus and affect millions of women worldwide. These benign tumors can cause a range of symptoms, from heavy menstrual bleeding and pelvic pain to reproductive issues. For many years, hysterectomy, the surgical removal of the uterus, was the primary treatment option for women with severe fibroid symptoms. However, in recent years, a less invasive alternative has gained popularity – Uterine Fibroid Embolization (UFE). In this blog, we will explore uterine fibroids, their impact on women’s health, and why UFE may be a preferable treatment option over hysterectomy.
Understanding Uterine Fibroids
Uterine fibroids, also known as leiomyomas or myomas, are noncancerous growths of the uterine muscle. They can vary in size, from tiny seedlings to large, grapefruit-sized masses. While some women may have fibroids and never experience symptoms, others can suffer a wide range of problems that significantly impact their quality of life. Common symptoms include:
- Heavy menstrual bleeding
- Pelvic pain and pressure
- Frequent urination
- Pain during intercourse
- Lower backache
- Infertility or recurrent miscarriages
These symptoms can be debilitating, affecting a woman’s physical and emotional well-being. Historically, when fibroids caused severe symptoms or other complications, a hysterectomy was often recommended as the ultimate solution.
Hysterectomy vs. Uterine Fibroid Embolization (UFE)
Hysterectomy involves the complete removal of the uterus, making it an effective treatment for uterine fibroids. However, it is a major surgery with long recovery times, potential complications, and irreversible consequences. For many women, the prospect of losing their uterus, and thereby their ability to conceive and bear children, can be emotionally distressing. Additionally, the recovery period for a hysterectomy can be several weeks, impacting work, family life, and overall well-being.
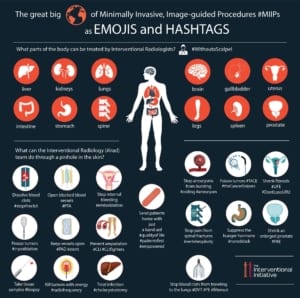
Uterine Fibroid Embolization, on the other hand, offers a minimally invasive alternative. This procedure, also known as UFE, involves a radiologist inserting a tiny catheter into the blood vessels supplying the fibroids. Small particles are then injected through the catheter to block the blood flow to the fibroids, causing them to shrink and die. UFE is performed under local anesthesia, often on an outpatient basis, with a significantly shorter recovery time compared to hysterectomy.
Advantages of Uterine Fibroid Embolization (UFE)
- Preservation of Fertility: One of the most significant advantages of UFE is that it allows women to preserve their fertility. Unlike hysterectomy, where the uterus is removed, UFE merely shrinks the fibroids, leaving the uterus intact. This is crucial for women who wish to have children in the future.
- Minimally Invasive: UFE is a minimally invasive procedure that avoids large abdominal incisions. This leads to reduced pain, shorter hospital stays, and a faster recovery compared to the more invasive hysterectomy.
- No Hormonal Changes: Hysterectomy can trigger hormonal changes, leading to early menopause. UFE doesn’t interfere with hormonal function, allowing women to maintain their natural hormonal balance.
- Effective Symptom Relief: UFE is highly effective in relieving fibroid symptoms, with studies showing that over 85% of women experience significant improvement.
- Reduced Risk: Since UFE doesn’t involve major surgery, it comes with fewer risks of infection, excessive bleeding, and other surgical complications.
- Cost-Effective: UFE tends to be more cost-effective than hysterectomy, considering the shorter hospital stay and recovery time.
Uterine fibroids can significantly impact a woman’s quality of life, causing distressing symptoms and reproductive issues. While hysterectomy has long been the standard treatment, Uterine Fibroid Embolization (UFE) offers a compelling alternative for women who wish to avoid the irreversible consequences of hysterectomy. UFE is minimally invasive, preserves fertility, and provides effective symptom relief.
Ultimately, the choice between UFE and hysterectomy depends on the individual circumstances, the severity of fibroid symptoms, and the patient’s reproductive goals. Consulting with a board-certified interventional radiologist at Radiology of Indiana to discuss the available options is crucial for making an informed decision regarding the most suitable treatment for uterine fibroids. To learn more visit radiologyofindiana.com or call (317) 621-5555.