A Closer Look at Varicose Veins
Varicose veins are a bothersome problem that many of us know little about. This familiar yet undiscussed condition affects one in three adults, yet most patients don’t seek proper treatment. Join us as we take a closer look at varicose veins!
Understanding Varicose Veins – What Are They?
When circulatory system vessels have become abnormally or excessively dilated, it’s known as varicose veins. While more commonly experienced in women, it can affect anyone, with approximately 23% of adults living with it. Varicose veins appear as blue-green twisted or bulging lines beneath the skin’s surface. The veins become enlarged when the valves in the veins no longer function properly and can’t return deoxygenated blood to the heart. As a result, stagnant blood accumulates in portions of the leg veins resulting in pressure buildup and their characteristic swollen appearance. While primarily found in the legs, they can appear elsewhere on the body, such as the feet.
How to Recognize Varicose Veins
Various factors contribute to the formation of varicose veins—genetics, sedentary lifestyle, extended periods of standing, hormonal changes, and even excessive exposure to the sun. A common myth surrounding varicose veins is that treatment is pursued solely for cosmetic reasons. However, this could not be further from the truth. This condition can cause many downright painful symptoms.
The most common symptoms include:
- Aching or burning sensations when standing
- Discoloration around veins
- Swelling of the ankles and legs
Remember the power of good habits for those fearful of developing varicose veins. Proper care, such as regular exercise, lots of water, weight management, and elevated legs while resting, can minimize your risk for varicose veins. A healthy diet, compression stockings, and the limitation of alcohol are also highly advised.
When to Worry About Varicose Veins
While often harmless, you should seek medical attention if you experience severe symptoms such as intense pain or itching around the veins. Also, look for other signs of complications, such as sores that ooze fluid or bleeding directly from a vein. It’s important to note that varicose veins increase the risk of deep venous thrombosis (DVT) or blood clots. Varicose veins can also decrease mobility and interfere with everyday activities, so it’s vital to remain vigilant of symptoms.
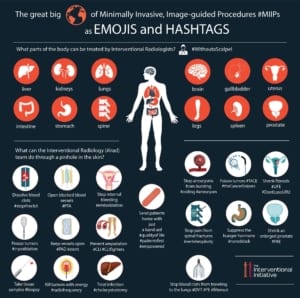
The Role of Interventional Radiology in Treatment
At Radiology of Indiana, we often favor a form of treatment known as Endovenous Laser Ablation due to its efficacy with our patients, with a success rate of approximately 98%. In the past, a surgical procedure known as vein stripping that consisted of entirely removing the vein from the leg was most common. Yet, with the emergence of endovenous laser therapy, surgery is no longer necessary. This speedy procedure will have you walking in and out of our office within an hour, as it does not require general anesthesia. This minimally invasive procedure uses laser energy to seal off problematic varicose veins. By inserting a small laser fiber into a vein through a tiny needle, the laser energy can heat the vein walls and collapse it closed. Covered by all insurance types, treatment options such as endovenous laser ablation are available for those diagnosed with symptomatic varicose veins.
It’s important to note that interventional radiology offers varied treatment options. The best action plan for you can be achieved by scheduling an appointment today. Through radiology, patients can find relief from this painful condition.
 To learn more about interventional radiology services for varicose veins, visit our website or contact us at 317-621-5555 today!
To learn more about interventional radiology services for varicose veins, visit our website or contact us at 317-621-5555 today!
Resources:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/varicose-veins